Identifying HIE: an overview#
Executive summary
Identify cases of HIE
Challenges:
In clinical practice, it is difficult to identify the cause of NE, requiring careful clinical phenotyping.
The definition of HIE has varied significantly, and terminology often blurred with neonatal encephalopathy
It is difficult to quantify the severity of HIE
Examples of how HIE is identified elsewhere:
Neonatal Data Analysis Unit - either diagnosis code for NE or HIE, or therapeutic hypothermia for 2+ days
ACOG-AAP task force - HIE more likely if: Apgar-5 and Apgar-10 < 5; Umbilical artery pH <7 and/or base deficit >= 12mmol/L; Multiple organ dysfunction; Neuroimaging evidence; Presence of sentinel hypoxic or ischaemic event; Abnormal FHR; Spastic Quadriplegia or Dyskinetic Cerebral Palsy; Other causes ruled out
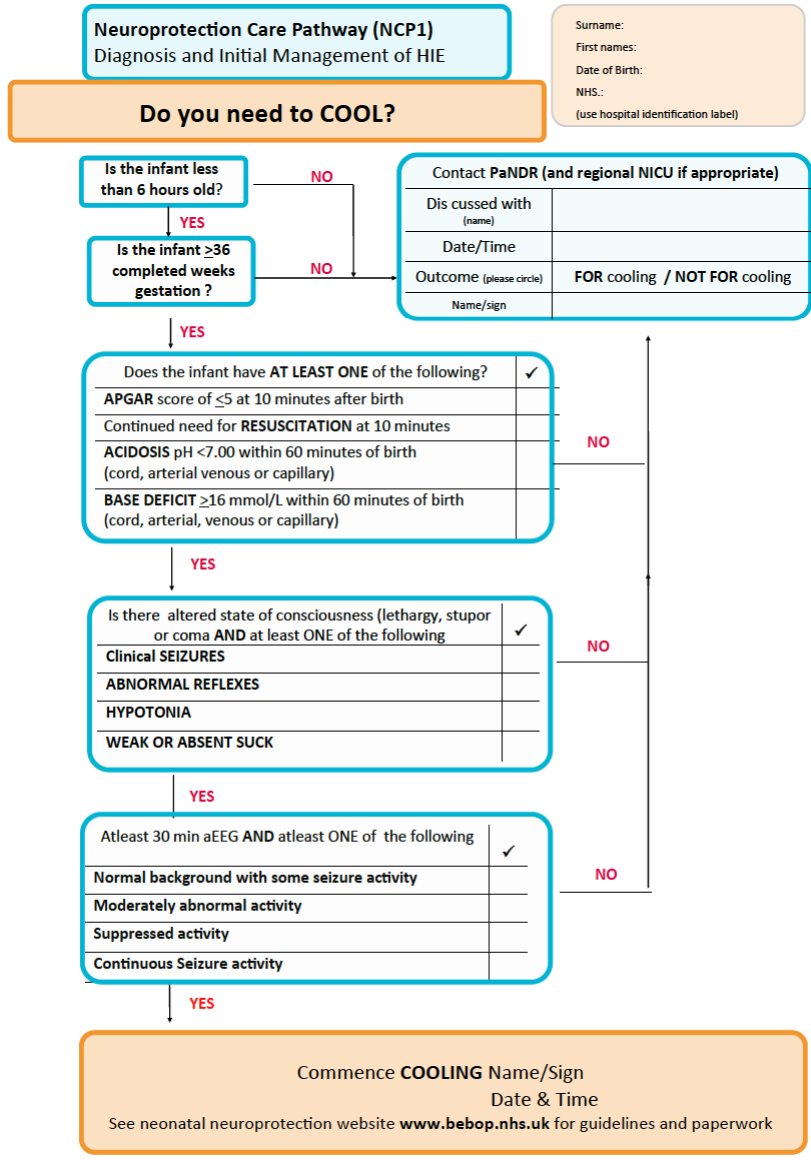
Criteria for therapeutic hypothermia - (a) one of Apgar-10 <=5, continued need resuscitation at 10min, pH<7, or base deficit >= 16mmol/L; (b) altered state of consciousness (lethargy, stupor, or coma) and one of: seizures, abnormal reflexes, hypotonia, weak/absent suck; (c) 30min aEEG with abnormal, supressed or seizure activity
Kurinczuk et al. 2010, and Ellenberg and Nelson 2012 - HIE identified based on presence of sentinel event like uterine rupture, major placental abruption, or cord prolapse (and not features that are not specific to hypoxia ischaemia)
The following pages provide further information on some of the indicators for HIE that are suggested above including indicators that are:
Standalone: Therapeutic hypothermia, diagnostic code for HIE, sentinel event
Combination (i.e. often used in combination with others):
Hypoxia - umbilical cord blood gas, sentinel event, resuscitation, meconium
Brain injury - transfer to neonatal care services, cerebral palsy diagnosis, neuroimaging evidence, symptoms of neonatal encephalopathy
Both - Apgar
Not recommended: Death, abnormal CTG
Why is it difficult?#
There are several challenges when it comes to diagnosing HIE, and defining a strategy for identifying it from patient data. These are as follows…
#1: It is difficult to identify the cause of neonatal encephalopathy. Identifying the precise causal pathway is often challenging.
‘It is difficult to prove the presence of cerebral hypoxic ischemia with the exception of well characterized animal models and particular cases of neonatal stroke.’ [Molloy and Bearer 2018] ‘Careful clinical phenotyping may help differentiation of NE by cause. This requires examination of the obstetric course and fetal monitoring records; careful and repeated neurological examination; early multichannel EEG or aEEG recordings of background brain activity; MRI and ultrasound brain imaging; and microbiological, biochemical and genetic analysis to rule out sepsis, inborn errors of metabolism, or epileptic encephalopathies, where indicated’.[DEFiNE - Molloy et al. 2023]
‘As such, many prominent bodies, including the American Academy of Pediatrics and the British Association of Perinatal Medicine (BAPM), advocate for using NE until the exact aetiology is determined.’[COHESION - Quirke et al. 2013] This means that using descriptive terminology like NE is preferable in the newborn period, before workup and course are known, rather than an etiology-based definition like HIE, which implies a single known etiology.[DEFiNE - Molloy et al. 2023] Clinical categorization, such as NE caused by sepsis, genetic causes, stroke, or those with a multifocal origin is required to ensure targeted management where possible for non-HIE causes.[DEFiNE - Molloy et al. 2023]
#2: There is not a consensus definition/set of diagnostic criteria for HIE.
‘An international evidence-based consensus is required to define NE, classify the subgroups, and their diagnostic criteria.’ The DEFiNE group has ‘developed a protocol for a consensus definition of NE. The evidence synthesis has started with a systematic review of definitions of NE used in randomized controlled trials involving patients with NE. This has revealed a huge disparity between, and little consensus on, definitions of NE. The next stage is to complete a protocol for a study to develop an international and multidisciplinary consensus definition using a modified Delphi consensus approach. The Delphi approach is an iterative process with repeated rounds of evaluation and voting to help determine consensus among a group of experts and parents with different levels of knowledge and expertise. We will use an online real-time Delphi approach to arrive at a consensus definition.’[DEFiNE - Molloy et al. 2023]
It is also important that a consensus definition is reached for mild HE, which has been variably defined. This is particular as the risk/benefit of providing therapeutic hypothermia to mild NE is not yet well characterised and trials are required.[DEFiNE - Molloy et al. 2023]
#3: There has often been blurring between neonatal encephalopathy and hypoxic ischaemic encephalopathy.
The definition for neonatal encephalopathy (as presented on the last page) does not does not specify subgroups, etiology, or guide management. This ambiguity has been criticised as hindering case definition, collaborative research, and data synthesis and confusing families and caregivers.[DEFiNE - Molloy et al. 2023]
Moreover, the terms “neonatal encephalopathy” and “hypoxic ischaemic encephalopathy” have often been used interchangeably, which is misleading, as HIE is actually a sub-group of NE. In practice, NE can occassionally be mistaked for HIE at birth. Also, congential neuromuscular disorders can be mistaken for NE (if they are disorders that involve abnormal tone,movements, and respiratory insufficiency).[DEFiNE - Molloy et al. 2023] Chalak et al. 2019 support this, stating that diagnosis of HIE or asphyxia is often over-utilised in practice and not clinically justified by the limited data at birth.[Chalak et al. 2019]
A systematic review of 67 RCTs from 1998 to 2022 found notable variation in terminology - 56/67 referred to HIE, whilst 16 referred to NE - and yet the most common inclusion criteria were not necessarily specific to HIE - Apgar scores, metabolic acidosis, reduced level of consciousness, reduced tone, and abnormal reflexes.[COHESION - Quirke et al. 2013]
#4: It is also difficult to quantify the dose, duration and severity of hypoxia ischaemia. [DEFiNE - Molloy et al. 2023]
Why does it matter?#
It is beneficial to understand the aetiology of NE. It can lead to the development of targeted adjunctive therapies related to the underlying mechanism and development of preventative strategies.[Chalak et al. 2019] ‘NE could be stratified by etiology. Subclassification and consensus definition will allow better collaboration and development of appropriate therapies for each subgroup, as a single “magic bullet” therapy is unlikely to treat all potential causes of NE.’[DEFiNE - Molloy et al. 2023]
It is also important when we might do harm by attributing a cause (e.g. hypoxia ischemia) to the disorder (encephalopathy).[Chalak et al. 2019]
Clear diagnosis is crucial for parents to help them to access accurate prognostic information and support.[DEFiNE - Molloy et al. 2023]
An early diagnosis is also crucial - as, for example, treatment with therapeutic hypothermia must be within the first six hours of injury for optimum benefit.[COHESION - Quirke et al. 2013]
Examples for how HIE has previously been identified#
Example 1. Neonatal Data Analysis Unit and the Department of Health#
The Department of Health commissioned the Neonatal Data Analysis Unit (NDAU) at Imperial College London to extract data from the National Neonatal Research Database (NNRD) and to calculate annual rates for Brain injuries occurring during or soon after birth for England from 2010 to 2015.
As part of this work, they had to develop a definition and methodology for identifying brain injury. This group defined brain injuries occurring during or soon after birth as follows:
Population - all babies admitted to a neonatal unit
Time period after birth - all brain injuries detected during neonatal unit stay
Conditions included -
Signs consistent with neonatal encephalopathy in term or near term infants (altered tone, altered consciousness, seizures)
Caveat: They found that data on signs of NE were not consistent over time - the fields used to define “altered tone” and “altered consciousness” only began from October 2010 onwards. Therefore, for this project, they dropped those and just looked for “seizures”.
Diagnosis of intracranial haemorrhage, perinatal stroke, hypoxic ischaemic encephalopathy (HIE), central nervous system infection, or kernicterus (bilirubin encephalopathy) in any infants
Preterm white matter disease (periventricular leukomalacia) in pre-term infants
Denominator - all live births
Exclusions - congenital encephalopathies (including inborn errors of metabolism), congenital infections, and congenital brain abnormalities
They also decide on a definition for HIE. In the briefing paper circulated before their meeting, they note that the current definition used by Each Baby Counts (Royal College of Obstetricians and Gynaecologists national quality improvement programme) is:
Greater than or equal to 37 weeks gestation at birth
Any of the following diagnosis codes entered into Diagnosis at discharge field:
Severe Hypoxic Ischaemic Encephalopathy (HIE)
Severe Neonatal Encephalopathy
Grade 3 Hypoxic Ischaemic Encephalopathy (HIE)
OR meet one of the following criteria from daily variables, within first 7 days:
Decreased central tone and comatose and seizures
Received therapeutic hypothermia (cooling)
Receiving diagnosis (daily data variable) of severe (grade 3) Hypoxic Ischaemic Encephalopathy (HIE)
They note that defining HIE by treatment means:
It will include infants who do not develop detectable brain injury
It may discourage use of treatment in borderline cases
In the briefing paper, they offer some options of definitions to be considered, for HIE these were:
Daily variables observed within first 72 hours, and therapeutic hypothermia needs to be received for 3 consecutive days
The decision decided upon in their consensus meeting for HIE was:
Diagnosis of NE or HIE (severe, moderate, grade 2 or grade 3)
Therapeutic hypothermia for 2 or more consecutive days
Example 2. Definition of HIE from the American College of Obstetrics, Gynecology, and Pediatrics (ACOG-AAP) Task Force#
The American Colleges of Obstetrics, Gynecology, and Pediatrics (ACOG-AAP) task force defined HIE as a restrospectively designated diagnosis - i.e. you start with a diagnosis of NE and then subsequency - based on accumulated evidence - subclassify it as HIE. They make recommendations - although recognise that ‘knowledge gaps still preclude a definitive test or set of markers that accurately identifies, with high sensitivity and specificity, an infant in whom neonatal encephalopathy is attributable to an acute intrapartum event’. Their latest recommended assessment for HIE is [American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy 2014]. Prior recommendations include that detailed in [Hankins and Speet 2003].
Recommendation for neonatal encephalopathy:
Born at or beyond 35 weeks
Manifested by a subnormal level of consciousness or seizures, and often accompanied by difficulty with initiating and maintaining respiration and depression of tone and reflexes.
Attributing cause to hypoxia ischaemia: ‘In confirmed cases of neonatal encephalopathy, the following assessment will determine the likelihood that an acute peripartum or intrapartum event was a contributor. This list is based on the premise that neonatal encephalopathy that is due to acute hypoxia–ischemia will be accompanied by abnormal neonatal signs and be associated with contributing events in close temporal proximity to labor and delivery. The goal of the assessment is to compile a constellation of markers concerning neonatal status, contributing events, and developmental outcome to determine if they are consistent with acute hypoxia–ischemia and may not be explained by other etiologies. Thus, when more of the elements from each of the item categories are met, it becomes increasingly more likely that peripartum or intrapartum hypoxia–ischemia played a role in the pathogenesis of neonatal encephalopathy.’ [American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy 2014]
Recommendation for neonatal signs consistent with hypoxia-iscahemia
*Apgar-5 and Apgar-10 less than 5 (and unlikely if Apgar-5 greater than or equal to 7)
Fetal umbilical artery pH less than 7 and/or base deficit greater than or equal to 12 mmol/L (and unlikely if pH >7.20)
Neuroimaging evidence of acute brain injury with MRI or magnetic resonance spectroscopy, consistent with hypoxia ischaemia
Multiple organ dysfunction [American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy 2014]
Recommendation for type and timing of contributing factors that are consistent with hypoxia-ischaemia:
Sential hypoxic or ischaemic event just before or during labour and delivery (A ruptured uterus Severe abruptio placentae Umbilical cord prolapse Amniotic fluid embolus with coincident severe and prolonged maternal hypotension and hypoxemia Maternal cardiovascular collapse Fetal exsanguination from either vasa previa or massive fetomaternal hemorrhage)
Fetal heart rate (FHR) patterns consistent with hypoxia ischaemia - (a) category II fetal heart rate pattern lasting 60 minutes or more that was identified on initial presentation with persistently minimal or absent variability and lacking accelerations, even in the absence of decelerations (b) Category I fetal heart rate pattern that converts to Category III (c) Additional fetal heart rate patterns that develop after a Category I fetal heart rate pattern on presentation, which may suggest intrapartum timing of a hypoxic–ischemic event, include tachycardia with recurrent decelerations and persistent minimal variability with recurrent decelerations
Neuroimaging evidence on timing and type of brain injury patterns - e.g. there are several well-defined patterns of brain injury and their evolution on MRI that are typical of hypoxic–ischemic cerebral injury in the newborn, including deep nuclear gray matter or watershed cortical injury. If a different pattern of brain injury or evolution of injury exists on MRI, then alternative diagnoses should be actively pursued (eg, metabolic and genetic investigations).
*No evidence of other proximal or distal factors that could be contributing - in the presence of other significant risk factors—such as abnormal fetal growth, maternal infection, fetomaternal hemorrhage, neonatal sepsis, and chronic placental lesions—an acute intrapartum event as the sole underlying pathogenesis of neonatal encephalopathy becomes much less likely.
*Spastic Quadriplegia or Dyskinetic Cerebral Palsy - other subtypes of cerebral palsy are less likely to be associated with acute intrapartum hypoxic–ischemic events - and other developmental abnormalities may occur, but they are not specific to acute intrapartum hypoxic–ischemic encephalopathy and may arise from a variety of other causes [American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy 2014]
Molloy et al. 2023 note that this definition may exclude some cases of HIE due to factors like:
Milder acidosis
Higher Apgar scores
Non-classical patterns of injury on MRI
Progressive, subacute evolution of HIE
Incomplete data, such as outcomes that do not include severe motor deficit
Incomplete data collection[DEFiNE - Molloy et al. 2023]
Example 3. Criteria for decision to deliver therapeutic hypothermia#
These are detailed more on the therapeutic hypothermia page, but the image below is the criteria for cooling, copied from the NHS East of England Guidelines for Management of Infants with Suspected HIE. Hence, this is the criteria typically used in the NHS shortly after birth, to determine whether an infant is likely to have HIE, based on the information available to them at the time.
Example 4. Kurinczuk et al. 2010, and Ellenberg and Nelson 2012#
Kurinczuk et al. 2010 wrote a best practice guideline on epidemiology of neonatal encephalopathy and hypoxic–ischaemic encephalopathy. Ellenberg and Nelson 2012 conducted a review of studies on intrapartum risks of cerebral palsy.
Kurinczuk et al. 2010 state - with reference to the ACOP-AAP 2002 - that HIE should just be used to define a sub-set of cases of NE where there is evidence of a recent, usually intrapartum, hypoxic ischaemic cause of the NE.[Kurinczuk et al. 2010] This refers to the occurence of sentinel events like uterine rupture, major placental abruption, or cord prolapse.[Ellenberg and Nelson 2012]
Typically, the presence of indirect clinical markers alongside features of encephalopathy are used to imply occurence of hypoxia ischaemia. However, they argue that you should use NEITHER of these - so NOT…
Findings that could result from a variety of etiologic factors like abnormal fetal heart rate or meconium in the amniotic fluid.
Signs of brain injury itself (seizures, encephalopathy)
The former is in the context of stating that seizures or encephalopathy are evidence that hypoxia-ischaemia occurred and was the cause. This is because uses those features in that way produces a tautological situation due to circular reasoning - that (a) presence of injury is marker that intrapartum complications occurred, and (b) presence of injury is the consequence of those complications - and so, it reaffirms the assumed connections between intrapartum events and NE, since the features were used to identify cases and to define NE. These signs of brain injury are clinical features, and don’t reflect the underlying cause as being hypoxia. [Kurinczuk et al. 2010] [Ellenberg and Nelson 2012]
Steve Thornton highlighted that the findings of Kurinczuk et al. 2010, and Ellenberg and Nelson 2012 are very important.
However, it is worth being aware that 10-36% HIE cases have a recognised sentinel event (as on sentinel event page).
Indicators of HIE#
As above, attempts to diagnose/define/identify HIE are varied, with several different indicators used. I have explored these indicators (and others that have been mentioned or used elsewhere) in the following pages, and summarised below. This should be read in the context of the recommendations above, such as those from the Neonatal Data Analysis Unit and the Task Force. The method of identifying HIE could involve a single indicator or combintions (AND / OR) of indicators.
Standalone indicators#
Therapeutic hypothermia: Alone, this outcome is specific to HIE and should capture moderate to severe HIE cases. Requires consideration of whether certain units would be more likely to treat certain infants (either over time, or who don’t meet the accepted criteria). Do be aware though that use of this as an outcome means that your definition of HIE is that criteria used to decide whether infants require cooling.
Diagnostic codes for HIE - A French validation suggested half of infants coded with HIE were false positive, and that over a third of infants with HIE were not identified. Uncertain for English data, or for codes beyond ICD P91.6.
Sentinel events
Combination indicators#
Combination of indicators for hypoxia and encephalopathy (some combination of which would’ve been used by the person who decided HIE occurred above). I’ve attempted to divide them into indicators of hypoxia v.s. encephalopathy - but many of these are often thought of quite blurrily (limitations of which are pointed out on last page).
Indicators that hypoxia occurred:
Umbilical cord blood gas analysis - Must (a) consider metabolic acidosis, (b) not require low pH (as many infants with HIE won’t have low pH), and (c) not base decision only on low pH (as many infants with low pH won’t have HIE)
Steve Thornton: “I think cord blood gases are a better indicator than implied in your text (if low).”
Sentinel events
Resuscitation - Resuscitation (e.g. mechanical ventilation, CPR, adrenaline) is often required in infants with HIE and infants who receive therapeutic hypothermia. However, not all infants need it, and not all infants who need it will have HIE, so should not use alone as an indicator. You might focus on a particular type of resuscitation - e.g. mechanical ventilation. Intubation may also be used as part of resuscitation (but no longer an indicator for meconium at delivery, as newborns are no longer intubated for this)
Meconium-stained amniotic fluid - Various possible causes. Associated with HIE.
Steve Thornton: “Meconium is a weak indicator”
Indicators for brain injury:
Transfer to neonatal care services - Alone, this is not suitable as 95%+ of admitted infants will not have HIE. However, in combination with other indicators of HIE, it could support identifying more unwell infants with HIE (most unwell, if focussed on NICU).
Cerebral palsy diagnosis - Spastic or dyskinetic Cerebral Palsy is an important outcome in the context of HIE. However, not all HIE cases will lead to cerebral palsy, and HIE is not the only possible cause of cerebral palsy.
Neuroimaging evidence consistent with HIE - Not certain whether this data would be available, and whether it would be in a format we could interpret (i.e. without knowledge of MRI, just notes with conclusions of professional). Would definitely indicate brain injury occurred. Not certain whether it distinguishes cause of injury (i.e. HIE different patterns to NE of other causes) - but there are patterns typical of HIE infants, so it does help support the case for HIE in that sense.
Steve Thornton: “Neuro imaging is really helpful, but it needs correct interpretation and my feeling is that often the local reports do not reflect expert opinion.” “I think that neuro imaging can distinguish between HIE, and other causes, but I am not a neuroradiologist.”
Symptoms of neonatal encephalopathy
Often used for both:
Apgar scores - The Apgar score is used to assess the status of a newborn immediately after birth and whether they are responding to resuscitation. It is repeatedly stated that it should not be considered to be (a) evidence of asphyxia, or (b) a consequence of asphyxia, or (c) to predict outcomes - even if it is associated with higher likelihood of HIE. However, it is often used.
Not recommended#
Death - Death is an outcome that can result from HIE - however, it doesn’t help us identify whether or not an infant had HIE.
Abnormal CTG - The high intra- and inter-observer variability in interpretation, likely minimal record of decision in records, and challenges in automated interpretation (and challenges of even getting that data) - along with the fact that this can have high false positive and false negative - mean I wouldn’t recommend this.
Steve Thornton: Agrees that CTG is not recommended
