Therapeutic hypothermia#
Executive summary
Outcome: Administration of therapeutic hypothermia.
Specific to HIE?
Yes - this is a treatment only administered to infants with suspected HIE
Which infants with HIE?
Current guidance is that this is for treatment of infants with moderate to severe HIE meeting criteria of (a) Less than 6 hours old (b) 36 weeks gestation or older (c) Apgar, resuscitation, pH, base deficit, (d) Altered state of consciousness or coma, and seizues, abnormal reflexes, hypotonia, or weak or absent suck (e) 30min amplitude integrated electroencephalography (aEEG) and abnormal/seizure/suppressed activity
However, a survey of UK neonatal units found 74% would offer from 33-35 weeks gestation, 74% would offer to infants with post-natal collapse, 56% would offer to infants between 6 and 24 hours from birth, 35% would offer to infants with mild HIE (note: there is no widely accepted definition of mild encephalopathy and criteria to identify it vary among clinicians), and 5% would offer to infants with surgical conditions
Any other benefits or caveats not already mentioned?
Some units offered it in 2000s (inconsistent across country), but NICE guidance recommending use came out in 2010, and became more widespread use by 2011 - so there will be change over time and across the country in use
Will include infants who do not go on to develop detectable brain injury
Conclusion: Recommended. Alone, this outcome is specific to HIE and should capture moderate to severe HIE cases. Requires consideration of whether certain units would be more likely to treat certain infants (either over time, or who don’t meet the accepted criteria). Do be aware though that use of this as an outcome means that your definition of HIE is that criteria used to decide whether infants require cooling.
What is it?#
‘Therapeutic hypothermia (or “cooling”) is currently the only neuroprotective treatment that has been proven to reduce death and neurological sequelae in term infants with moderate to severe HIE.’ It must be started within 6 hours of birth.[source]
‘Hypothermia treatment is delivered through either selective head or whole body cooling of the infant… decreasing the infant’s body temperature to between 33°C and 36.5°C. Infants are generally cooled for 48 to 72 hours and then rewarmed slowly to prevent complications (e.g., hypotension).’[source]
It works by minimising ‘the production of toxic substances that can cause brain injury. When the brain does not have enough oxygen or energy to function, it produces toxic chemicals which can ultimately damage a baby’s brain. When oxygen is restored to the brain, there is a time period where the brain attempts to recover from the injury. Unfortunately, a second wave of toxic chemicals is often released, which can further injure the brain. Because of this, the majority of brain damage can occur during and after restoration of blood flow and oxygen to the brain – not necessarily during birth. Once the cooling therapy is completed, we slowly warm the baby back up to inhibit the production of additional chemicals and reduce the risk of brain damage.’[source]
Effectiveness#
‘A Cochrane systematic review of 11 randomised controlled trials has shown this therapy reduces death and neurodisability in infants with moderate to severe encephalopathy. Despite 46% of infants having developed adverse events related to cooling, it is now the standard treatment for neonatal encephalopathy in high-income countries (HiCs).’[COHESION - Quirke et al. 2013]
‘Many infants still experience adverse outcomes despite cooling, including cerebral palsy (CP), cognitive, visual or hearing impairment, and even death. Moreover, a significant proportion of infants with mild HIE, who are currently not eligible for therapeutic hypothermia, have an adverse outcome at follow-up.’[source]
‘The recent HELIX (hypothermia for moderate or severe neonatal encephalopathy in low-income and middle-income countries) study showed that not only did therapeutic hypothermia not decrease the combined outcome of death or disability in India, Sri Lanka, and Bangladesh, it significantly increased mortality alone’.[DEFiNE - Molloy et al. 2023] As a result, treatments are now being investigated as stand-alone treatments or adjuvants to therapeutic hypothermia (e.g. erythropoietin, darbepoetin).[COHESION - Quirke et al. 2013]
When was it introduced?#
‘In January 1998, Marianne Thoresen and Andrew Whitelaw established a laboratory and clinical research programme at the University of Bristol and UH Bristol to investigate and develop therapeutic hypothermia as a treatment for neonatal HIE.’[source]
There have been three versions of the Cochrane review - 2003, 2007 and 2013.[source]
In 2007, there was a survey of neonatal units on access to and opinions of therapeutic hypothermia:
Access to therapeutic hypothermia was widespread but not universal - it existed in 55% of units, and 41% of units offered transfer to a regional unit for therapeutic hypothermia
57% of survey respondents thought it was effective or very effective - 43% felt more data was needed [source]
NICE guidance recommending therapeutic hypothemia for neonates with hypoxic perinatal brain injury was published in May 2010 [source] - this new guidance stated there was sufficient evidence on the safety and efficacy of therapeutic hypothermia “to support the use of this procedure in carefully selected neonates…”.[source]
‘By 2010/11, therapeutic cooling had been adopted as standard treatment.’[source]
Criteria for cooling#
The image below is the criteria for cooling, copied from the NHS East of England Guidelines for Management of Infants with Suspected HIE. You can observe that these include:
Less than 6 hours old
36 weeks gestation or older
Apgar, resuscitation, pH, base deficit
Altered state of consciousness or coma, and seizues, abnormal reflexes, hypotonia, or weak or absent suck
30min amplitude integrated electroencephalography (aEEG) - an aEEG is a trend analysis of 1-2 channels of EEG, and visual patterns allow the reviewer to assess the severity of encepahlopathy and to monitor for seizures [Abend et al. 2011] - and abnormal activity, suppressed activity or seizure activity.
These are the TOBY guidance, and they are followed by the vast majority of NICUs in the UK.[source]
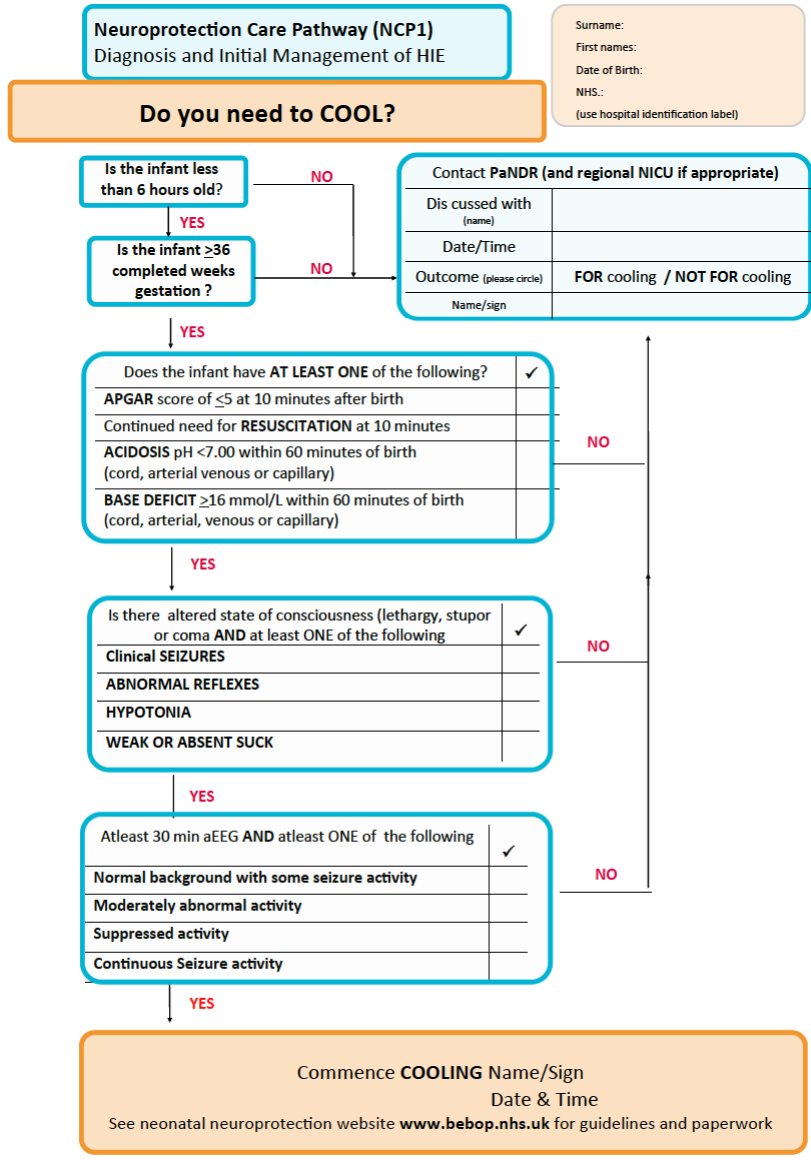
The criteria are also detailed in [Mosalli 2012].
Therapeutic creep#
In recent years, there has been a therapeutic creep, where therapeutic hypothermia is offered outside the currently accepted cooling criteria. These ‘grey case scenarios’ could potentially benefit from cooling but literature available is minimal. A survey of UK units asked whether they offer cooling to these infants, with percentages below -
Late pre-term infants (74.4%, n=32) - none of the published RCTs included infants less than 36 weeks gestation - anecdotally, cooling centres offer to babies from 33-35 weeks gestation - and there is currently a large RCT in this age group (Preemie Hypothermia for Neonatal Encephalopathy study: NCT01330576)
Infants with mild HIE (34.8%, n=15) - there is no widely accepted definition of mild encephalopathy and criteria to identify it vary among clinicians
Infants with postnatal collapse (PNC) (74.4%, n=32) - PNC is rare with high mortality rate and severe neurodevelopmental compromise for survivors
Infants identified between 6 and 24 hours (55.8%, n=24) - review did not indicate favourable or harmful results from late cooling
Infants with surgical conditions (4.6%, n=2) - these infants were not included in trials due to concerns about significant complications (wound healing, cardiovascular compromise, coagulopathy)
Other considerations#
Defining HIE using treatment (cooling) will include infants who do not go on to develop detectable brain injury.[Gale et al. 2017]
