Meconium-stained amniotic fluid#
Executive summary
Outcome: Meconium-stained amniotic fluid (MSAF)
Specific to HIE?
No - MSAF associated with gestational age, hypoxia, infection, and otherwise unknown cause
Which infants with HIE?
Varying figures - 7% to 20% of infants with meconium had pH<7 (or <=)
Any other benefits or caveats not already mentioned?
NA
Conclusion: Potentially recommended. Various possible causes. Associated with HIE.
Meconium-stained amniotic fluid#
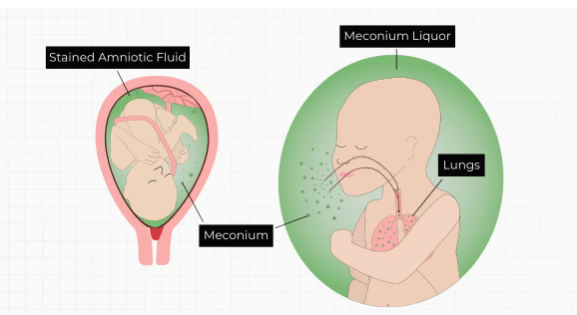
Meconium is the first feces of the newborn and is typically sticky and greenish-yellowish-black. If this happens in utero (whilst the baby is still in the womb), the meconium can get into the amniotic fluid (the liquid surrounding the fetus).
Meconium-stained amniotic fluid (MSAF) ‘occurs in 5 to 20% deliveries at term’ and is considered a risk factor for several different neonatal complications including:
Neonatal hypoxic-ischemic encephalopathy
Neonatal sepsis
Neonatal seizures
Meconium aspiration syndrome (MAS) - respiratory distress in infants with MSAF that can’t otherwise be explained - only developed by 5% infants exposed to MSAF
Cerebral palsy
Figure from [source]:
Association with HIE#
‘The largest study to examine the relationship between MSAF and fetal acidemia included 42,709 term pregnancies, of which 8136 had MSAF. Meconium was associated with a significantly higher rate of umbilical artery pH ≤7.00 (7% [56/8136] vs 3% [95/34,573]; P<.001; odds ratio [OR], 2.5; 95% confidence interval [CI], 1.8–3.4).’
‘However, most neonates born to mothers with MSAF do not have evidence of metabolic acidemia at birth. Indeed, in a recent retrospective study including 3590 deliveries, MSAF was not associated with umbilical artery acidemia, and 80% of neonates with MSAF had a pH ≥7.20.’
‘These conflicting results between the 2 largest studies may be explained by differences in the use of intrapartum fetal heart rate monitoring. In the first study, surveillance was performed with intermittent auscultation, whereas in the second study, continuous electronic fetal heart rate monitoring was used. It is possible that improved surveillance allows earlier detection of a compromised fetus, and thus the association between MSAF and umbilical artery acidemia was not observed.’
‘It is widely accepted that fetal hypoxia leads to meconium passage. However, experimental studies have challenged this view. For example, maternal aortic constriction in pregnant rabbits to induce fetal distress is not associated with meconium passage, and neither is acute hypoxia of pregnant sheep sufficient to drop the fetal partial pressure of oxygen. Similarly, repeated cord occlusion leading to fetal acidemia is not associated with meconium passage in fetal sheep. A role for the autonomic nervous system in the regulation of pathologic fetal defecation has been proposed. Indeed, sympathetic system blockade, achieved chemically with 6-hydroxydopamine, in the same experimental paradigm of cord occlusion does lead to meconium passage. It is also noteworthy that normal fetal defecation in animal studies is observed in the absence of fetal hypoxemia or acidemia.’
Other associations with meconium#
Defecation in utero is a physiological phenomenon. Factors associated with MSAF are:
Gestational age - rate of MASF increases with gestational age, can reach 27% at 42 weeks of gestation
Hypoxia - MSAF has been associated with fetal acidemia and chronic hypoxia
Intraamniotic infection/inflammation - MSAF is associated with microbial invasion of the amniotic cavity in term and preterm gestations
‘In the absence of these 3 factors, the etiology remains unknown.’
